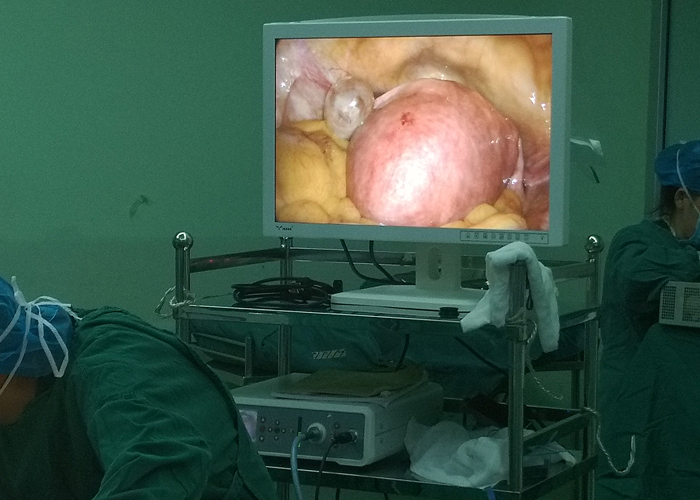
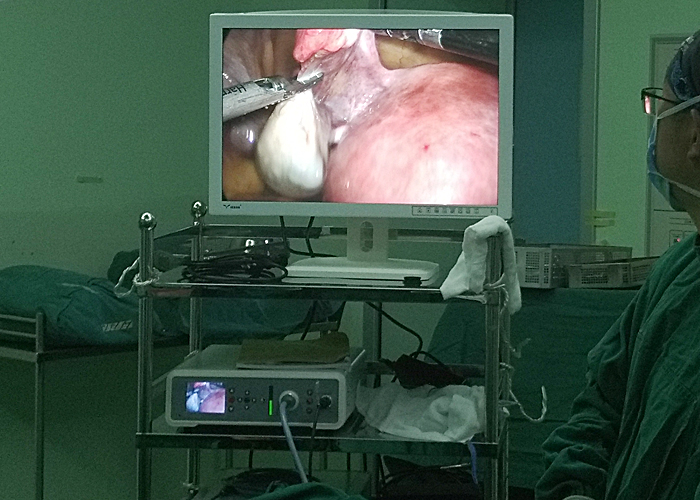
Laparoscopic cholecystectomy (LC) involves inserting a special catheter into the peritoneal cavity and injecting about 2-5 liters of carbon dioxide. After reaching a certain pressure, 4 small holes of 0.5-1.5 cm are made in the abdomen to dissect the gallbladder triangle. Structure, cut off and clamp the cystic duct and cystic artery, and then remove the entire gallbladder including the stones. If the gallbladder is too large, the gallbladder can be moved to the puncture port of the abdominal wall, the gallbladder can be cut open, the aspirator can suck out the bile, or the stone can be taken out. After the gallbladder collapses, it can be taken out of the body. Then, under the laparoscopic operation, the gallbladder was carefully and carefully removed.
Indications for laparoscopic cholecystectomy:
1. Symptomatic gallbladder diseases: gallbladder stones, gallbladder polyps, chronic cholecystitis, early acute cholecystitis, etc.
2. Asymptomatic gallbladder disease with comorbidities: accompanied by diabetes, cardiopulmonary dysfunction, stable stage,
3. Gallbladder diseases that easily cause gallbladder cancer: gallbladder stones older than 60 years old, huge stones (diameter> 2cm), ceramic gallbladder, single gallbladder polyps with diameter> 1cm, fast-growing gallbladder polyps, wide base polyps, gallbladder neck Department of polyps and so on.
Laparoscopic cholecystectomy is not suitable for people:
Absolute contraindications
1. Accompanied by severe cardiopulmonary insufficiency and unable to tolerate anesthesia, pneumoperitoneum and surgery.
2. Those with coagulation dysfunction.
3. Acute cholecystitis with severe complications, such as gallbladder gangrene and perforation.
4. Acute severe cholangitis or acute gallstone pancreatitis.
5. Gallbladder cancer or gallbladder bulging lesions are suspected to be gallbladder cancer.
6. Chronic atrophic cholecystitis, gallbladder volume <4.5cm×1.5cm, wall thickness>0.5cm (measured by B-ultrasound).
7. Severe liver cirrhosis with portal hypertension.
8. In the middle and late stages of pregnancy.
9. Accompanied by abdominal cavity infection, peritonitis.
10. Those with diaphragmatic hernia.
Relative contraindications
1. Acute exacerbation of calculous cholecystitis.
2. Chronic atrophic calculous cholecystitis.
3. Common bile duct stones and obstructive jaundice.
4. Mirizzi syndrome, stone incarceration in the neck of the gallbladder.
5. Previous history of upper abdominal surgery.
6. Morbid obesity.
The general steps of the operation:
① Create pneumoperitoneum.
②Establish operation holes.
③Treat the gallbladder triangle.
④ Strip the gallbladder.
⑤Remove the gallbladder.
⑥ Eliminate pneumoperitoneum.
Precautions for laparoscopic cholecystectomy:
1. Precautions when creating a pneumoperitoneum
When performing abdominal wall puncture on obese patients, the two breakthrough feelings are not obvious. To confirm that the needle tip is indeed in the abdominal cavity, connect the syringe with saline to the insufflation needle. If you see the saline in the syringe naturally flow in with gravity Abdominal cavity, indicating that the puncture needle has entered the abdominal cavity at this time. Always watch the gas flowmeter when inflating. The pressure should not exceed 13mmHg at 4L/min. The abdomen will bulge evenly during inflation and the liver dullness will disappear.
After the pneumoperitoneum is established, in order to further confirm whether the umbilical has intestinal adhesions, a Palmer suction test can be done: connect a 10ml syringe with saline to an 18-gauge needle, and penetrate into the abdominal cavity through the umbilicus. At this time, the dioxide in the abdominal cavity Carbonized gas pushes the saline from the syringe outwards, and only gas enters the needle, indicating that there is no intestinal tube here. If blood or fluid cannot be drawn out, it means local adhesions. If intestinal juice is drawn out, it means intestinal adhesions.
2. Precautions for the use of high-frequency electric knife
In laparoscopic organ injuries, the common bile duct and intestinal duct accidentally injured by electrosurgery are the most common. Attention should be paid to:
(1) The insulating layer of laparoscopic instruments such as electrocoagulation hooks should be intact and replaced in time when damaged; ②Preoperative preparations should be sufficient, and enema should be performed to eliminate intestinal flatulence; ③Using low-voltage and high-frequency electrocoagulation, at 200V It is safe, and no ionizing spark should be generated during cutting; ④The surgeon often fails to find the injury of the intestine at the time, so the electrocoagulation device should always be placed in the monitoring screen during the operation; ⑤When the surgeon uses the electrocoagulation hook , The force should be kept upward (abdominal wall) to prevent the electrocoagulation hook from rebounding and burning the surrounding organs.
3. Dissecting Calot's Triangle
Mainly to prevent bile duct damage. Anatomical abnormalities of the bile duct are common, so be especially careful. Electrocoagulation should not be used during the dissection to prevent damage to the common bile duct. It is best to use only the electrocoagulation hook or separating forceps for careful dissection. When the triangle adhesion is very serious or congestion and edema are obvious, and the common bile duct is unclear, it should be promptly converted to open surgery.
4. Deal with the cystic duct
One of the reasons for the occurrence of biliary fistula is the improper treatment of the cystic duct. Short or thick cystic duct, incomplete clamping of the titanium clip, often makes the treatment of the cystic duct difficult. When encountering a shorter cystic duct, try to clamp the titanium clip on the side of the common bile duct to open the side of the gallbladder and drain the bile. The broken end of the cystic duct should have enough length to prevent the titanium clip from slipping off. When encountering a thicker cystic duct, ligate it with silk thread first, and then attach the titanium clip. There are large-sized titanium clips that have a better effect on thicker cystic ducts.
5. Intraoperative cholangiography
There are many methods of angiography during biliary tract surgery. Our method is to clamp the cystic duct on the side of the gallbladder first, then cut a small opening in the cystic duct, and insert a tube from the outer edge of the rectus abdominis muscle. The ureter is used as a catheter and inserted about 3 cm. The opening of the cannula is clamped with fixed forceps. Contrast agent is injected to take pictures. Laparoscopy is used for monitoring during the operation. There are special forceps for radiography, which is very convenient to use.
6. Remove the gallbladder
The abdominal muscles of the umbilical cannula are relatively weak and easy to separate with a hemostatic forceps. When the gallbladder stones are large, first lift the gallbladder neck out of the abdominal wall, open the gallbladder to suck up the bile, and use stone-removing forceps to remove the stones from the gallbladder. If the stone is large, it can be crushed in the gallbladder before being removed. After removal, it should be stained with blood and bile in the incision. Do not pull out forcefully when the incision is not large enough to cause a ruptured gallbladder stone to fall into the abdominal cavity. If any stones fall into the abdominal cavity, they should be taken out as many as possible, otherwise the remaining stones will cause abdominal cavity infection and adhesions.
7. Pay attention to recording the procedure
Laparoscopic cholecystectomy is a potentially dangerous operation. The whole process of the operation should be recorded and stored properly as a "black box" so that the cause can be found in the event of surgical complications.