Knee joint adhesions (alias: knee joint fibrotic adhesion, knee joint fibrous adhesion, knee joint fibrous stiffness, knee joint stiffness, knee joint stiffness, knee joint extension and flexion dysfunction) are serious injuries to the knee joint and around the joint and after surgery The serious complication is a very common and very troublesome clinical problem. Because the knee joint cannot be straightened and/or bent, it brings a lot of inconvenience to the patient's daily life, and affects the patient's life, psychological and social activities. Traditional incision and release surgery has large trauma and bleeding, which affects early postoperative recovery, and may form new adhesions after surgery, which affects the curative effect. However, the advent of arthroscopy makes it possible to loosen minimally invasive knee joint adhesions.
Arthroscopy lysis for the treatment of knee joint adhesions
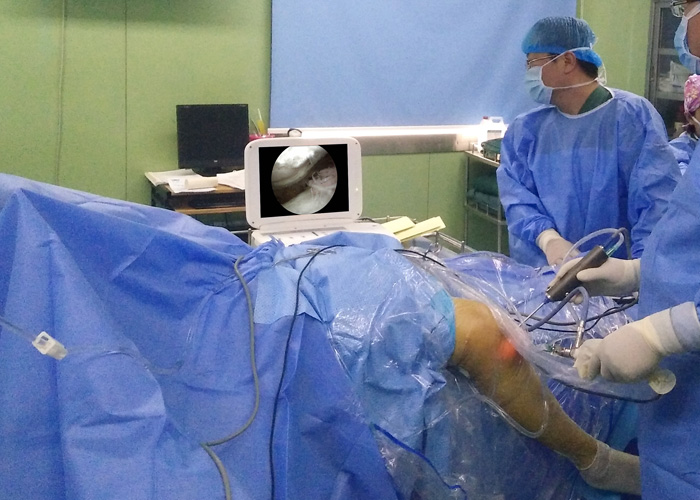
Surgical methods:
Adopt four 0.8cm incisions on the inner, outer and upper patella of the knee, first bluntly separate the lateral sulcus with a blunt puncture cone, separate about 20ml of space and insert a 4mm diameter, 30° arthroscopy. The sheath is continuously perfused and expanded with normal saline, and the sheath is sucked and washed intermittently. Enter the electric planer from the upper and outer entrance of the patella to remove the fiber scar bundles in the lateral groove, and gradually expand to the midline. When the tough fibers are encountered, they are cut with a push knife to remove the stump. It is often necessary to cut the inferior patella cord before entering the planing head, which can be loosened from the outside to the midline, including the expansion of the suprapatellar capsule; then use the same technique to expand the medial groove with a mirror and a planer. Extend to the midline until the sub-patella and suprapatellar capsule adhesions are completely removed; then the anterior internal and anterior external approach is used for intra-articular and external compartments and intercondylar fossa adhesions lysis. Under the microscope, it was found that due to long-term adhesion, the articular cartilage surface was uneven, softening and degeneration were obvious. Supplemented with light manual release, manual release and microscopic release and cleanup are performed alternately until the knee joint flexion reaches 110° or more, and the extension is 0°, and then a full cleanup and cartilage trimming are performed again. After the operation, the joint adhesion preventive agent was injected. The average operation time was 145 minutes, and 20,000 ml of normal saline was used for lavage. After the operation, the joint was suctioned with a No. 10 urinary catheter, and the knee was externally fixed with a plaster at 90°.
The advantages of arthroscopy lysis for the treatment of knee joint adhesions
Ankylotic knee joints have extensive adhesions in the suprapatellar capsule, bilateral grooves, internal and external compartments, and intercondylar fossa. Most patients also have contractures of extra-articular structures. Massage under anesthesia is likely to cause serious complications such as patella fracture, femoral condyle fracture, articular cartilage injury, and patellar ligament tear. If the knee is bent strongly without loosening, it will only open the anterior tibiofemoral space, instead of the femoral trochlear sliding on the tibial platform, so this method is not suitable for patients with severe knee joint adhesions. The arthroplasty and quadriceps femoris arthroplasty, which are widely used in the past, are very traumatic. Most patients often cannot tolerate the severe postoperative pain and cannot perform early functional exercises, which leads to recurrence of adhesions. This is an incision and lysis procedure. The main reason for poor efficacy; clinical observations have found that patients with a relatively high pain threshold often perform well. On the other hand, scarring and skin atrophy due to trauma and long-term joint stiffness. Due to the fear of skin necrosis at the incision, the soft tissue and skin cannot be sutured when the joint is fully flexed, and external fixation cannot be performed when the joint is fully flexed. These skin conditions also have a great impact on the final curative effect. Arthroscopic arthroscopic arthroscopic arthroscopic arthroscopic arthroscopy has less trauma and light postoperative pain, which provides good conditions for patients to perform early functional exercises; small incisions generally do not cause skin necrosis due to long-term limited mobility after surgery, and It can be fixed in the largest possible flexion position, so the curative effect is greatly improved compared with open surgery.
Under arthroscopic lysis, the image is magnified, which is more accurate than the operation under open direct vision. It can remove the adhesion band and prevent the occurrence of re-adhesion. At the same time, the condition of articular cartilage is checked and necessary trimming is carried out to improve joint function and slow down joint degeneration. Greatly beneficial. It is operated under arthroscopy from the medial and lateral sulcus, which can completely avoid accidental damage to cartilage, cruciate ligament and meniscus, and has high safety.

Indications for arthroscopy lysis:
In arthroscopic surgery, attention should be paid to the selection of patients. The indications are mainly for patients with adhesions in the knee joint. For those with adhesions of the quadriceps, other lysis and angioplasty should be supplemented; in addition, attention should be paid to the postoperative knee joint. The possibility of instability, the joint is stable in the state of joint adhesion, if there is a ligament injury, the joint may become unstable after it is loosened, and new problems may occur. In addition, during the operation, it was found that the cartilage of the adhesion joints had different degrees of degeneration, softening, and unevenness, especially for those patients who had a longer adhesion time. After joint lysis, the direction in which the joint friction and weight-bearing will make the cartilage develop, whether it is repaired or degenerated, remains to be further observed.